CTR’s isolved Benefits Administration System Has it All!
CTR’s isolved Benefits Administration System provides all of the key benefits administration functionality within one application that is built right within your payroll system.
CTR’s isolved Benefits Administration Offers:
The isolved Benefits Administration system will handle all of your ACA Tracking, ACA Compliance, and Year-End 1095-C and 1094-C Reporting.
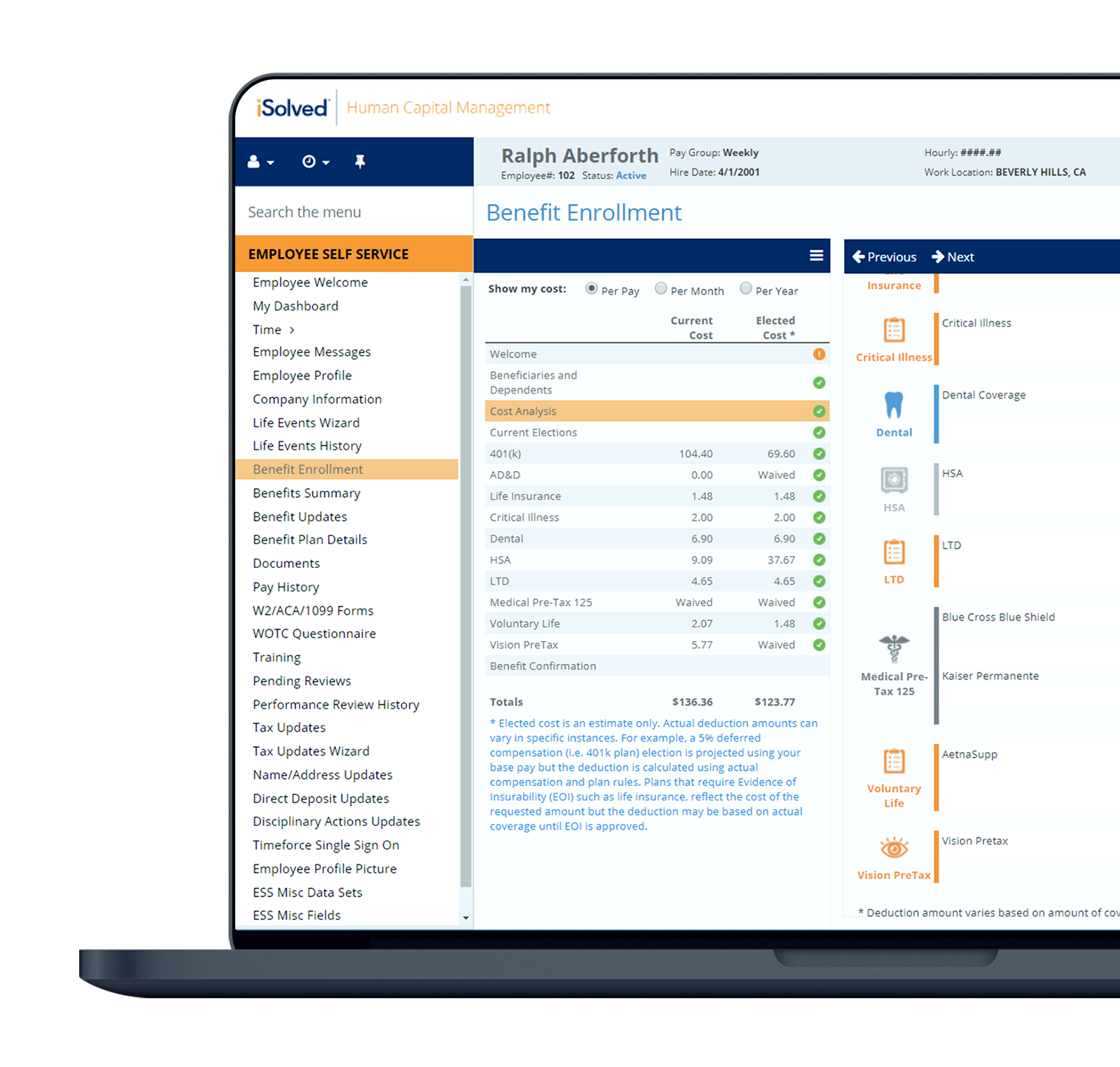
Employees can easily login and follow the step-by-step benefit enrollment wizard to complete their online enrollment. You can post employee messages, links to carriers, Plan Documents and Summary Plan Descriptions for employees to view and acknowledge.
isolved Carrier Connections let you choose the insurance carriers with which to integrate and send updates. Employers gain the benefits of timely and error-free enrollment updates, including elimination of error-related premium costs, an improved benefit usage experience and reduction of HR and IT workloads.
COBRA Administration is simple. When you terminate an employee in our system it triggers the appropriate COBRA notifications to be transmitted to your employees. A record of all transmitted COBRA documents is available right at your Fingertips within isolved.
Advantages of a Benefits Administration System
Your company is growing and your administrative team is struggling to keep up with the day-to-day benefits administration items for new enrollees and existing employees. There has been talk about evaluating a Benefit Administration System with an online employee benefit portal. As you embark on your journey you wonder whether an online enrollment tool is really worth the investment of time and money. Will it really save us time? Will our employees really use it?
Several studies have shown that Benefits Administration Systems have saved companies a tremendous amount of time. Still have some questions? Scroll down for some FAQs regarding Benefits Administration Systems.
Contact Us

What is the Best Benefits Administration System?
Now that you have determined that a Benefits Administration System is a fit for your organization, it’s time to begin the search for the best software.
You may be surprised to find the variety of options available to you. Everyone from your health insurance provider to your benefits broker and even your third-party administrator (if you have one) may have tools available. They may even pitch to you that the enrollment tool is “free” if you use their services. There is no doubt that benefit enrollment system will save your broker time, but the question is whether using your broker’s benefit enrollment tool will save your team time and effort—after all that is goal!
Your Benefits Administration Should Include All Steps of the Benefits Enrollment Process in One Application
Your team should determine what functions are available in the Benefits Administration System. The key is to ensure all benefits compliance functions are all available in one system to eliminate duplicate data entry. Key functionality that should be available in a benefits system should include the following items all within the same login and within the same application:
- COBRA Administration
- ACA Compliance
- ACA Tracking
- ACA Reporting
- Online Open Enrollment
- Benefit Eligibility Reporting
- Links to Carrier Websites
- Benefit Enrollment Alerts & Reminders
- Carrier Connections
Having a single source for all of these items will eliminate any additional data entry related to the benefits administration process.
Contact CTR for isolved Implementation and Support
Looking to learn a little more about isolved and how it can totally revolutionize your approach to HR? Contact us and we’ll get you in touch with one of our CTR specialists to help you discover how isolved can answer all your questions.